Eagles Syndrome
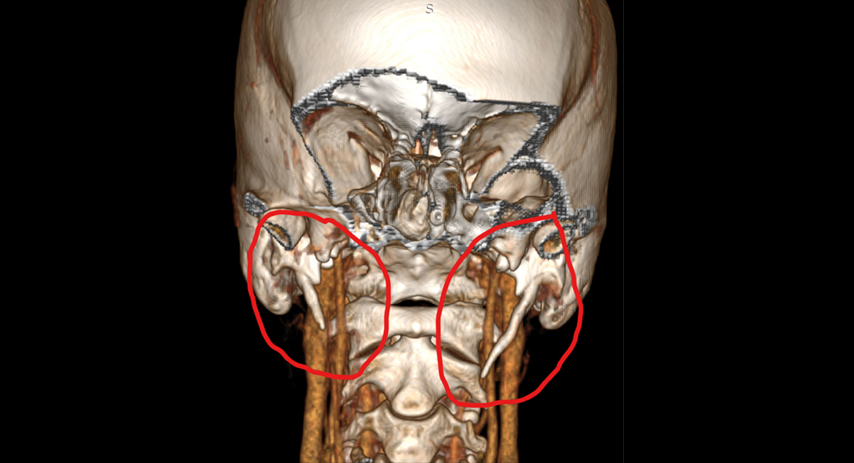
3D CT Angio of Dr. Victoria Perez
What Is Eagle Syndrome?
Eagle’s syndrome is a “rare” poorly understood condition that is believed to affect roughly 8% of the population. It is caused by a calcified stylohyoid ligament or an elongated styloid process which compresses nearby neurovascular structures. Please note that a “normal” length styloid process can also cause compression in certain cases. The standard for diagnosis is debatable among the medical community, leading to misdiagnosis over 80% of the time.
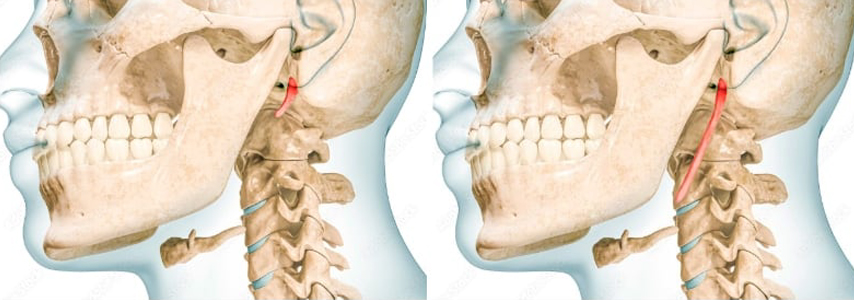
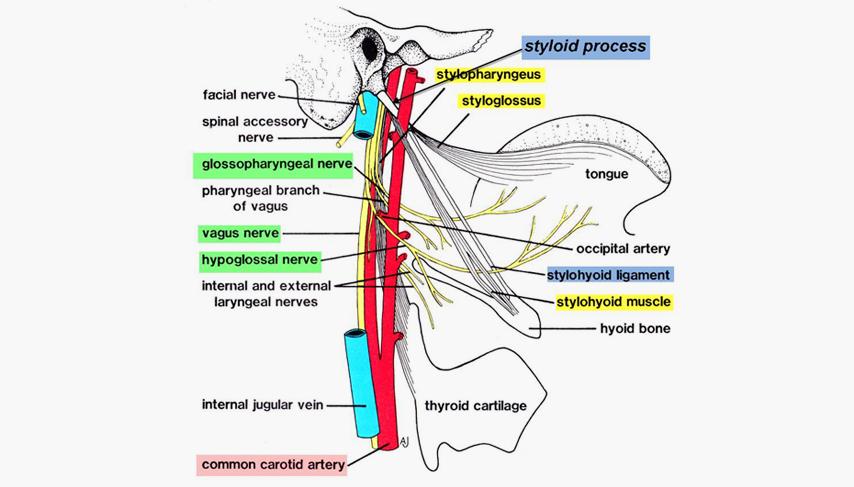
Neurovascular Compression
The internal carotid arteries and/or internal jugular veins can become compressed affecting blood flow into and out of the brain. Seven of the 12 cranial nerves can be directly affected with the other five being indirectly affected. Each nerve affected results in a different array of symptoms.
Cranial Nerves Most Commonly Affected by ES & Corresponding Symptoms:
Cranial Nerve V (Trigeminal nerve): Can cause facial pain particularly in the lower jaw region. Sinuses, teeth, eyes, nose and ears may all experience pain. All three branches can be affected.
Cranial Nerve VII (Facial nerve): Can cause facial pain, paresthesia, pressure & sometimes mild paralysis of eye lids, mouth, cheeks.
Cranial Nerve VIII (Vestibulocochlear Nerve): Less commonly implicated. This nerve may cause/contribute to dizziness.
Cranial Nerve IX (Glossopharyngeal nerve): The nerve most frequently affected. Its compression can cause throat pain/globus sensation, difficulty swallowing, pain/pressure/burning at the base of the tongue, First Bite Syndrome, palate pain/dysfunction, and referred ear pain.
Cranial Nerve X (Vagus nerve): Frequently affected. Can cause numerous symptoms, including difficulty swallowing, changes in voice, gastrointestinal problems, dizziness or fainting, breathing dysfunction, heart palpitations/heart rate changes, blood pressure irregularity, chronic cough, increased anxiety/depression, body temp dysregulation, and other debilitating symptoms.
Cranial Nerve XI (Accessory Nerve): Can cause pain/stiffness/swelling in the SCM, clavicles, & shoulders which can radiate down the arms.
Cranial Nerve XII (Hypoglossal Nerve): Can cause pain/burning or dysfunction of the tongue muscle.
Jugular Vein Compression (Internal Jugular Most Common) Symptoms:
Head and Neck: Headaches (from intracranial hypertension), neck pain and stiffness, dizziness, tinnitus/pulsatile tinnitus, hearing problems, neck discomfort.
Visual: Blurred or double vision, visual snow, afterimages, unstable visual field, distorted depth perception.
Neurological: Brain fog, difficulty focusing, anxiety, depression, dissociation, transient amnesia.
Carotid Artery Irritation/Compression (Internal Carotid Most Common):
Head and Neck: Headaches, memory loss/brain fog, confusion
Visual: Horner’s Syndrome, partial or full blindness – usually in one eye
Neurological: TIAs &/or strokes, numbness or tingling on half of body (usually upper half), speech impairment, chest pain/heart pain, neck pain
What are the “common” symptoms?
Facial/tooth pain
Ear pain /chronic tinnitus
Neck/ shoulder pain
Heart palpitations/ blood pressure changes/ orthostatic hypotension
Vocal loss
Migraines
Brain fog
Head & Ear pressure
Gastrointestinal problems
Cold and heat intolerance
Brain fog
Migraines
Hypo/Hyper Salivation
Head & Ear pressure
"Ice Pick" Ear pain
Vertigo/Off balance/ Rocking boat sensation
Difficulty swallowing/Sensation of something stuck in your throat/ Throat pain
Head & Ear pressure Feeling of impending doom/ "Irrational anxiety"
Ocular symptoms
Dry eye/ foreign body sensation
Excessive tearing
Double vision
Increased intraocular pressures/ Glaucoma
Transient ischemic attacks / Sudden vision loss
Ocular pain/ pressure
*This is not a comprehensive list. Symptoms are diverse due to the number of cranial nerves it can affect. The diffuse pain can be sharp, sudden, and nerve-like,
often triggered by swallowing, jaw movement, or head turning. THIS CONDITION IS MULTFACTORIAL and is known as the “MIMICKING DISEASE”
Common Misdiagnosis
Trigeminal Neuralgia- AKA “Suicide Disease”***
TMD/TMJ- Temporomandibular disorder***
Glossopharyngeal Neuralgia
Degenerative disc disease, Arthritis, Cervical spondylosis
Migraines
Dental cavities
Sinus headaches
Anxiety
Ernest syndrome
Tachycardia / Heart palpitations
- Ear Diseases- Meniere’s disease, Tinnitus- Vestibular migraines
What Causes Eagle Syndrome:
Whiplash/ neck trauma- Over 3 million cases in the US a year
Tonsillectomy- Over 530,000 tonsillectomies performed each year.
Cranial Cervical Instability***
Underling connective tissue disorders – Scoliosis, Ehler-Danlos Syndrome, Marfans, along with various Autoimmune conditions that attack connective tissue.
Teeth grinding/ clenching
Altering bite/jaw alignment
Hormone imbalances
DOWNWARDHEAD POSTURE… New epidemic is PHONE DEPENDANCE
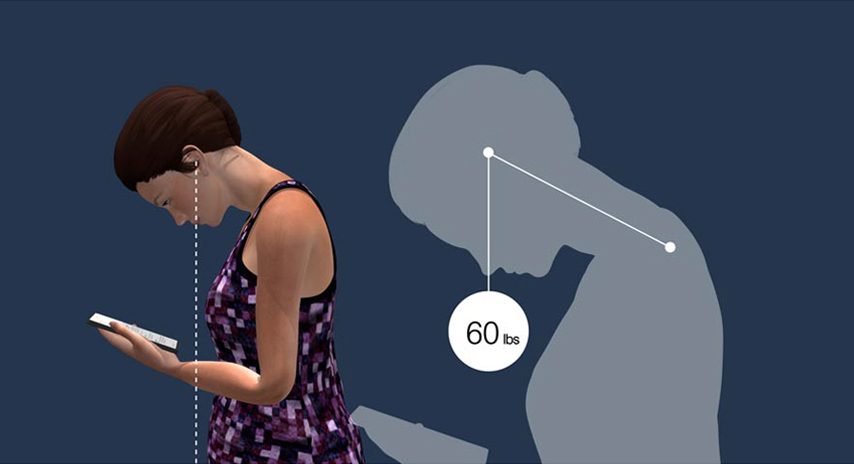
Downwardhead posture - Phone Dependance
Proper diagnosis/ Imaging
The gold standard for diagnosing ES is a CT scan of the head and neck with and without contrast. Dynamic testing is also beneficial. If vascular symptoms are present,
a CTA/V with contrast added at the arterial & venous phases of the heartbeat is best. Radiologists should assess styloid length, thickness and angle, and also look for any calcifications on the stylo-hyoid ligaments. Many doctors diagnose ES based on the length of calcification alone as opposed to considering patient symptomology or other styloid physiology such as angle of growth, thickness, how curved, pointed, or twisted the styloid is and other physical features which may dispose a normal length styloid to cause symptoms. To further assist in this critical diagnosis, Dr. Perez has established co-management care with radiology and can order proper CT imaging, after an initial consultation is established.
Treatment
Styloidectomy. Complete removal of the styloid process or calcification of the stylohyoid ligament. This condition is PROGRESSIVE and calcification will continue to grow if not fully resected. Most studies report a success rate between 80%- 90% for symptom relief after surgery.
Patient advocacy
https://livingwitheagle.org/
Please take the time to read the journeys of the thousands of patients looking for answers. Dr. Perez credits this forum for helping save her life.https://ohni.org/
Dr. Ryan Osborne is an internationally renowned expert in head and neck oncology as well as an Eagle's Syndrome specialist. Dr. Osborne conducted Dr. Perez’s styloidectomy and is accessible via virtual visits for consultations.
Misinformation and Challenges in Diagnosing Eagle Syndrome
Rarity and Lack of Awareness
Eagle syndrome is a relatively rare condition, making it less familiar to healthcare professionals in various fields.Non-Specific and Overlapping Symptoms
The overlap in symptoms can lead to misdiagnosis and delayed treatment as patients may seek help from various specialists without a definitive diagnosis.Challenges in Diagnosis
Although radiographic imaging, particularly 3D CT scans, can help confirm the diagnosis, it requires expertise in interpreting these scans and understanding the anatomical relationships of the styloid process.Limited Research and Expertise
There is a lack of robust statistical evidence and clear diagnostic criteria for Eagle Syndrome, making it difficult for healthcare professionals to establish a definitive diagnosisDelay in Diagnosis
Patients with Eagle Syndrome symptoms often experience significant delays in receiving a proper diagnosis, sometimes taking several years.
This delay can lead to frustration and emotional distress for patients as they go through multiple consultations and treatments without finding relief.

Dr. Perez shares her story
A failed healthcare system; My Journey to an Eagle Syndrome Diagnosis
Read her story3D CT-Angiography of Dr. Perez
“Atypical Neuralgia” misdiagnosis